December is supposed to feel magical, but for many women in their 40s and 50s, it’s the month when physical and emotional symptoms feel the strongest. Hot flashes flare under sweaters, sleep gets disrupted, mood swings intensify, and weight gain seems to happen overnight. It’s not your imagination — your hormones and the holiday season have a complicated relationship.
The good news is that small, realistic habits can help. Staying hydrated, increasing protein intake, going for short walks after meals, and enforcing a consistent bedtime can significantly improve how you feel. If your symptoms feel more intense than they used to, it may also be time for a hormone evaluation — especially if you’re noticing weight changes, mood swings, or sleep disruptions that don’t match your usual patterns.
With the right support, December doesn’t have to feel overwhelming. Understanding the hormonal shifts behind your symptoms is the first step toward feeling more like yourself — during the holidays and beyond.
Q’s
How fast will I feel better?
Many women notice improvements in hot flashes, sleep, and mood within 4–6 weeks, with continued gains as we fine-tune. (Lippincott Journals)
How long should I stay on HRT?
It’s individualized. Fracture protection and symptom relief last while you’re on therapy; benefits diminish after stopping, so we tailor duration and revisit yearly. (PubMed)
Ready to feel more like you again?
If perimenopause is disrupting your days (and nights), you don’t have to wait. Book a consultation to see if HRT is a good fit—get started.
A mental-health bonus
In a randomized clinical trial, transdermal estradiol plus intermittent micronized progesterone cut the risk of developing clinically significant depressive symptoms during the menopause transition by about half vs placebo over 12 months. (PMC)
References are studies that have been peer-reviewed & guideline sources.
- The Menopause Society (NAMS) 2022 Position Statement: HRT is the most effective therapy for vasomotor symptoms and GSM; prevents bone loss/fractures; benefit-risk depends on timing, type, dose, route. (Lippincott Journals)
- USPSTF 2022 Recommendation: Do not use menopausal hormone therapy for primary prevention of chronic conditions in postmenopausal persons. (uspreventiveservicestaskforce.org)
- ELITE Trial (NEJM 2016): Early (but not late) estradiol initiation slowed progression of subclinical atherosclerosis (CIMT). (New England Journal of Medicine)
- Fracture Reduction: WHI and other RCTs show reduced fracture risk during active use of HRT. (PubMed)
- Mood Benefit RCT (JAMA Psychiatry 2018): Transdermal estradiol + intermittent micronized progesterone prevented onset of clinically significant depressive symptoms in perimenopausal/early postmenopausal women. (PMC)
- WHI 18-Year Follow-Up (JAMA 2017): No increase in long-term all-cause mortality after 5–7 years of MHT vs placebo. (JAMA Network)
Recent Related Topics
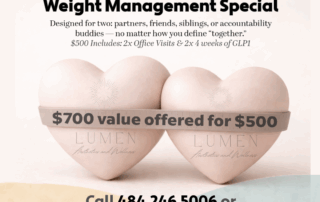
Better Together- A Valentine’s GLP1 Weight Management Special
Looking for a supportive, hormone-sensitive weight loss approach? Our 4-week GLP-1 therapy partner program helps reset metabolism safely and effectively.
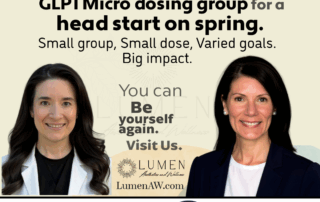
Microdose GLP-1 Metabolic Reset
Learn how a microdose GLP-1 can jump-start your metabolism, offering a gradual, comfortable approach to weight management.
From Fear to Facts – FDA to remove the “black box” safety warnings for HRT
What changed? On Nov 10, 2025, the FDA [...]
TrumpRX — GLP-1 Prices May Be Dropping — Here’s What We Know (So Far Today)
Today’s headlines point to lower out-of-pocket costs for GLP-1 [...]
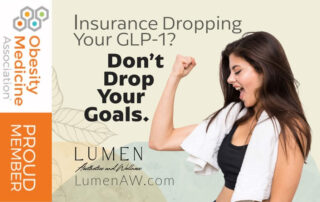
Insurance Dropping Your GLP-1?
When Coverage Changes, You Still Have Options - Don't [...]
Thinking about HRT?
Here’s Why “Sooner” Can Be Smarter. If your cycles [...]
Save on your consult.
$50 off your initial consultations for medical weight loss and/or hormone replacement therapy.
(Excluded from other specials)